VExUS in Cirrhosis
Earlier, we discussed the utility of POCUS in evaluating hemodynamic acute kidney injury in cirrhosis. The following images were obtained from a patient with alcoholic liver cirrhosis, who had been receiving empiric intravenous albumin at 1g/kg/day for four consecutive days due to acute kidney injury. Unfortunately, many healthcare providers fail to recognize the common occurrence of iatrogenic fluid overload and the diagnostic inadequacies of conventional physical examination. In this case, the continued administration of albumin was justified by pointing out the ‘absence of supplemental oxygen requirement’ and the presence of ‘chronic pedal edema’, both of which are poor markers of fluid status.
We decided to perform POCUS-enhanced physical examination. Lung ultrasound mostly revealed A-lines except for a few B-lines in the basolateral zones, which wasn’t too concerning. However, what about the right side of the circulation?
We then examined the inferior vena cava, which appeared plethoric, indicating elevated right atrial pressure. Due to challenging cardiac windows, diastolic parameters and stroke volume couldn’t be evaluated. Nonetheless, the parasternal long axis view revealed right ventricular dilation (recall the three musketeers post?). LVEF seems slightly reduced.




Obviously, the next step is VExUS –
The hepatic vein showed systolic wave reversal, suggesting severe congestion. It’s important to note that without simultaneous EKG, systolic reversal might be mistaken for a prominent A-wave. The notched pattern in the D-wave is probably due to delayed AV conduction. Interestingly, the patient’s recent outpatient echocardiogram from a few weeks ago did not reveal baseline structural tricuspid regurgitation. TR was mild at that time (but it’s quite likely that the TR worsened now).
Portal vein also demonstrates severe congestion with to-and-fro pattern, so does splenic vein.


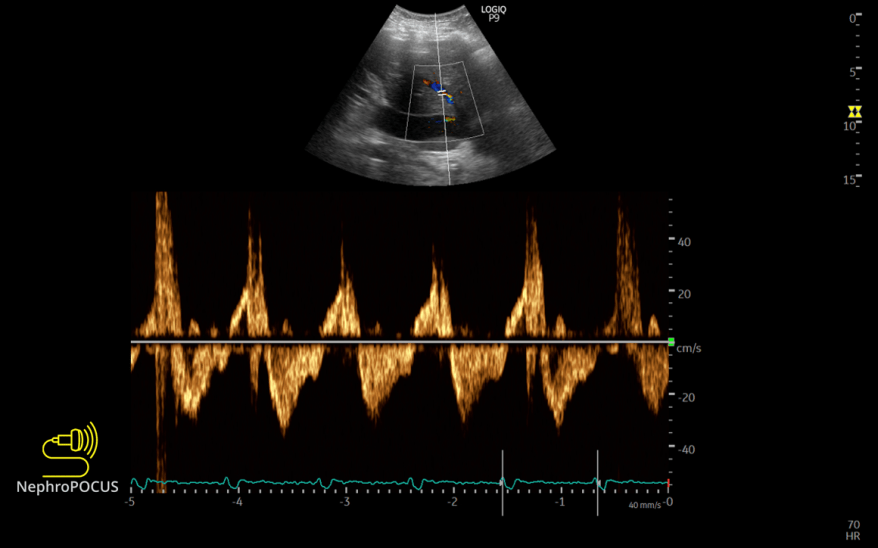
I do believe the waveforms above indicate venous congestion, although some might argue that liver vessels (specifically portal veins) are not reliable indicators in cirrhosis. Moreover, reduced RV function, worsening TR, delayed AV conduction can influence the hepatic S-wave amplitude. Therefore, we examined the intrarenal waveform, which clearly displayed a monophasic pattern (D-only below the baseline) with an elevated renal venous stasis index. Additionally, the femoral vein exhibited a pulsatile pattern, confirming systemic venous congestion as well as congestive nephropathy.


Furthermore, upon reviewing the right upper quadrant scan report from approximately a year ago, it read ‘Morphologic changes of cirrhosis’. ‘Patent hepatic vasculature with antegrade portal venous flow,’ suggesting that these flow changes are new, likely related to fluid overload.
Considering these POCUS findings, intravenous diuresis was advised in addition to stopping albumin. Within the next 24 hours, a negative fluid balance of 1.5 L was achieved, and the serum creatinine level improved from 3.4 mg/dL to 3.13 mg/dL. Follow-up POCUS couldn’t be performed as the patient was transferred to a different facility.
Point: Stop taking pride in precision guesswork and perform physical examination (POCUS-enhanced). Accurate diagnosis leads to better patient management regardless of it’s impact on mortality.
